Current study (published on 7 April 2021):
Vitamin D Resistance as a Possible Cause of Autoimmune Diseases:
A Hypothesis Confirmed by a Therapeutic High-Dose Vitamin D Protocol
Link to study
INFO FOR DOCTORS
Scientific principles
In this video, Dr Coimbra explains his work and research on ultra-high-dose vitamin D therapy in detail at the international Vitamin D Congress in 2018:
Dr Coimbra first put forward his theory of vitamin D resistance back in 2002 and has researched it both in his practice and in theory at the University of São Paulo. In 2013, he and his team published a study on using the Coimbra Protocol in patients with vitiligo and psoriasis. In it, he explained the scientific principles of the Coimbra Protocol’s effect on the immune system. The mode of action is identical for all autoimmune diseases, so Dr Coimbra claims that the same mode of action applies for all known diseases that stem from a derailment between the Th and Treg cells of the immune system.
Since then, more research has been conducted on the mechanism of vitamin D resistance and its activation. We know that single nucleotide polymorphisms (SNPs) can lead to problems with the synthesis, activation or binding of vitamin D to the cell receptor and to serious immune system disorders. The underlying principles of gene expression/epigenetics linked to vitamin D have been investigated by Prof. Carsten Carlberg, among others. In his work he demonstrated that some people need a much higher level of vitamin D in their blood to ensure healthy immune system function.
Extract from “A pilot study assessing the effect of prolonged administration of high daily doses of vitamin D on the clinical course of vitiligo and psoriasis”, Finamor, Coimbra et. al. 2013
(https://www.tandfonline.com/doi/full/10.4161/derm.24808)
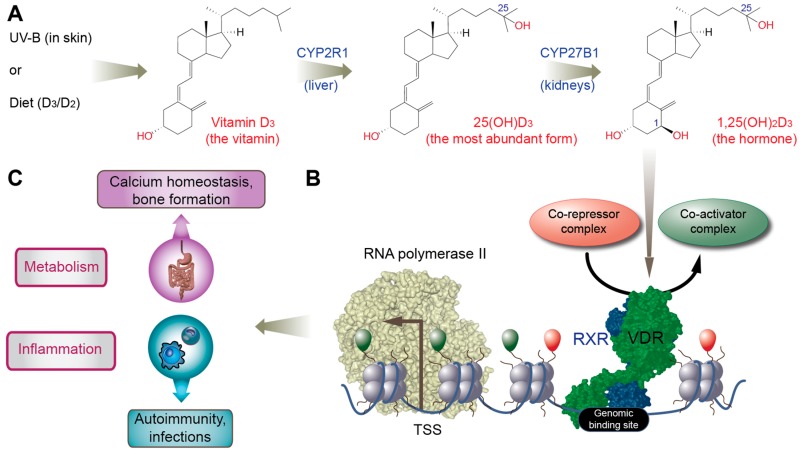
“The steroid hormone known as the active form of vitamin D (“calcitriol,” “1,25-dihydroxy vitamin D” or “1,25(OH)2D”) generates a wide range of biological responses. The human genome possesses 2,776 positions occupied by the [vitamin D receptor] VDR; about 10% of the human genes are, therefore, directly and/or indirectly responsive to vitamin D. Similarly, diverse human cells (including bone, colon, breast, prostate, skin, muscle, blood vessel, brain and immune cells) express the enzyme 25-hydroxyvitamin D-1 α-hydroxylase (CYP27B1), indicating that the extra-renal intracrine and paracrine 1,25(OH)2D3 [=calcitriol] synthesis may critically affect the activities of many tissues and organs. Accordingly, cumulative data have associated low vitamin D status (as assessed by measuring “25-hydroxyvitamin D3” or “25(OH)D3” [=calcidiol] – the main circulating form of vitamin D) not only to rickets and osteoporosis, but also to an increasing number of prevalent health disorders including autoimmune, infectious and cardiovascular diseases, hypertension, diabetes and deadly cancers.
Contrasting with the pathophysiological importance of 1,25(OH)2D3, vitamin D deficiency is a poorly recognized worldwide epidemic among both children and adults. Regular and moderate sun exposure (the only significant natural source of vitamin D for most subjects) is currently uncommon due to indoor lifestyle, sun avoidance and indiscriminate sunscreen use. Even though there is mounting evidence indicating that physiologic doses should be closer to those achieved through a few minutes of daily skin exposure to sunlight, the RDA upgraded (from 200 to 600 IU per day) by the Institute of Medicine in 2008 remains much lower than that, and are lower than the daily doses required to correct vitamin D deficiency in most subjects.
Higher daily doses may be particularly critical for controlling the activity of autoimmune disorders. Cumulative data over the past 30 y have established the regulatory effects of vitamin D on both innate and adaptive immune responses, and circulating levels of 25(OH)D3 inversely relate to the activity of autoimmune disease. Intracrine and paracrine actions of 1,25(OH)2D3 synthesized within immune cells may control inappropriate activation of interleukin-17-producing cells – the Th17 aberrant response, which may play a major pathogenic role in multiple inflammatory and autoimmune disorders. Cumulative evidence also indicates that vitamin D promotes—by both direct and indirect mechanisms – regulatory T cells (Treg) that inhibit a variety of inappropriate (both innate and adaptive) immune responses underlying autoimmune disease.
 Estimations of daily requirements of vitamin D3 for patients with autoimmune disorders should take account of the functional consequences of genetic polymorphisms related to vitamin D metabolism.
Estimations of daily requirements of vitamin D3 for patients with autoimmune disorders should take account of the functional consequences of genetic polymorphisms related to vitamin D metabolism.
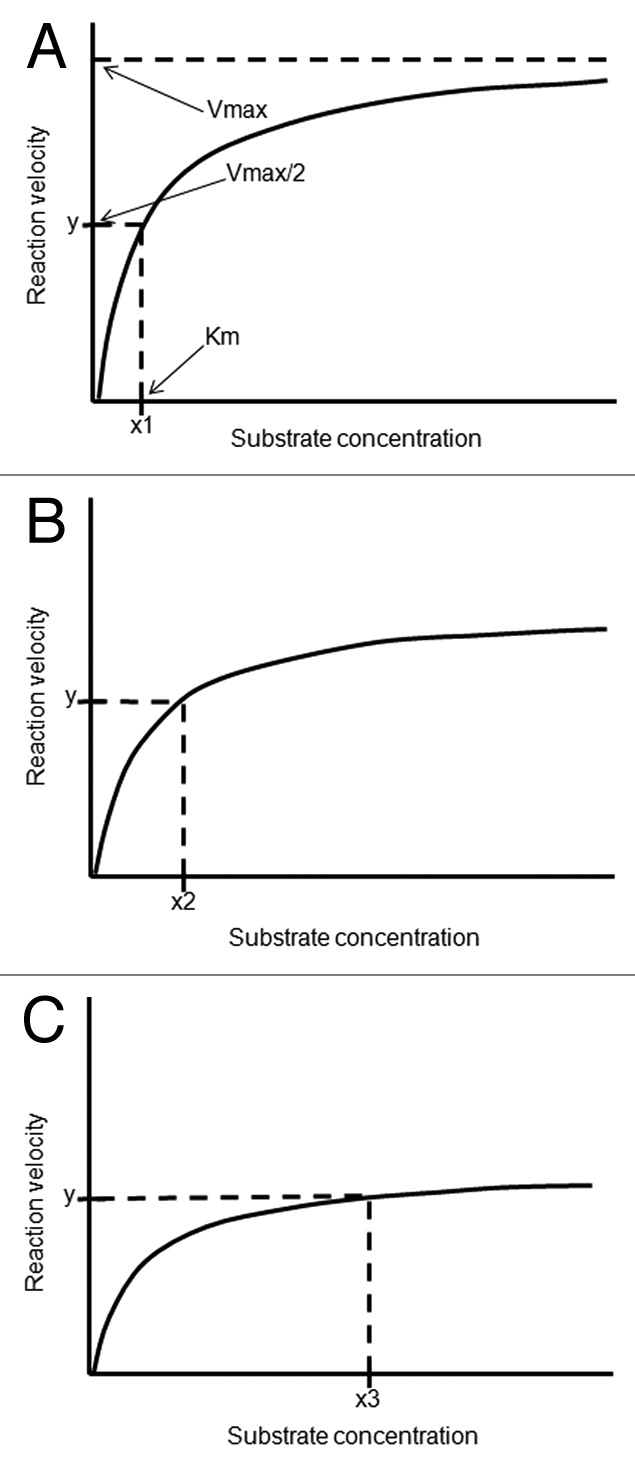
For instance, the polymorphic changes of the enzyme CYP27B1 associated with autoimmunity predictably originates a relative resistance to vitamin D, i.e. a higher level of circulating 25(OH)D3 [=calcidiol] required to achieve normal 1,25(OH)2D3 [calcitriol] concentrations within the immune cells. While the in vivo [Michaelis-Menten constant] Km of the normal enzyme exceeds the physiologic range of 25(OH)D3 concentrations, a polymorphic variant may have a higher Km (decreased affinity for substrate) and/or a lower Vmax [= maximal velocity of enzymatic reaction], requiring higher concentrations of substrate to achieve a physiologic rate of product formation.
Frequent genetic polymorphisms and wide (ten to a hundred fold) variability in enzyme expression of the cytochrome P450 superfamily of enzymes (CYPs) are common and may considerably modify enzyme activity, causing large interindividual variability in the rate of product formation. Therefore, a subject bearing a CYP27B1 polymorphism may be prone to develop autoimmunity for sustaining concentrations of 1,25(OH)2D3 within the immune cells that are insufficient for full intracrine and paracrine tolerogenic effects of this powerful steroid molecule. High doses of vitamin D3 leading to supraphysiologic range of circulating 25(OH)D3 may compensate for this genetic-related status of relative vitamin D deficiency, thereby establishing tolerance to auto-antigens.”
Publications and studies on vitamin D & autoimmune diseases:
- Vitamin D and Multiple Sclerosis: A Comprehensive Review, 2018:
Vitamin D and Multiple Sclerosis A Comprehensive Review.pdf - Role of gene polymorphisms in vitamin D metabolism and in multiple sclerosis.
Role_of_gene_polymorphisms_in_Vitamin_D_metabolism.pdf - Early stage study shows that vitamin D can promote myelin repair
Link zur Studie - Vitamin D supplementation in multiple sclerosis – Can be done something more?
Vitamin D in multiple sclerosis – Can be done something more.pdf - 1,25-(OH)2D3/Vitamin D receptor alleviates systemic lupus erythematosus by downregulating Skp2 and upregulating p27
Vitamin D receptor alleviates systemic lupus erythematosus.pdf - Immunomodulatory and Immunosuppressive roles of 1α,25(OH)2D3 in Autoimmune Diseases
Immunomodulatory and Immunosuppressive roles of 1α,25(OH)2D3.pdf - Modulatory Effects of 1,25-Dihydroxyvitamin D3 on Human B Cell Differentiation
Modulatory Effects of 1,25-Dihydroxyvitamin.pdf - Nutrigenomics of Vitamin D, C. Carlberg 2019
Nutrigenomics of Vitamin D, C.Carlberg 2019.pdf